Our sweet consumption habits may offer momentary joy, but there are a host of implications that come along with it. While the threats posed by sugar to our general health are widely recognized, a lesser-known adversary which is just as impacted by this pervasive ingredient is our dental health. The impact of sugar on our oral health is multifold. It causes dental issues like plaque and cavities, largely due to a series of biochemical reactions that sugar undergoes in our mouth. This discourse aims to shed light on the negative impacts of sugar on teeth. We ponder upon things as minuscule as bacteria to as intricate as our oral pH and saliva.
Biochemical reactions of Sugar and Oral Bacteria
The Complex Interplay of Dietary Sugars and Oral Bacteria: A Gate to Dental Pathologies
Biochemical pathways in the human body are often intricately interwoven, routinely fostering symbiotic relations that are essential for maintaining an optimal physiological balance. One such critical relationship exists between dietary sugars, oral bacteria, and the radiating implications on dental health. A detailed understanding of these tripartite biological dynamics has pivotal implications for preventive dentistry and oral health.
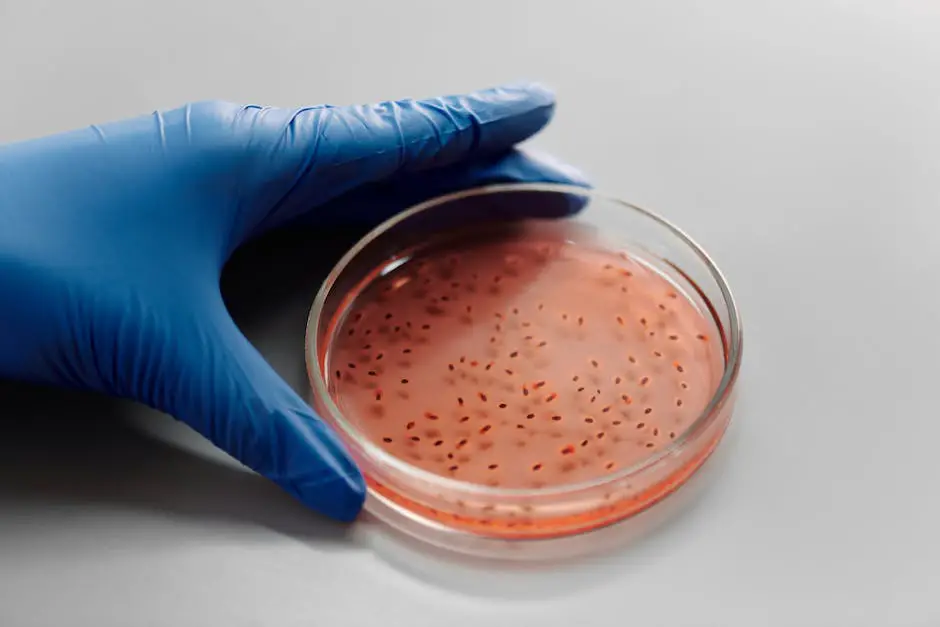
In the oral ecosystem, over 700 bacterial species cohabitate, with some contributing to oral health and others potentially precipitating dental problems. Our focus in this discourse zeros into Streptococcus mutans and Streptococcus sobrinus, two primary bacterial strains recognized for their contributory roles in tooth decay.
Dietary carbohydrates, most notably sugars, are the primary source of energy for Streptococcus strains. Upon consumption of sugar-rich foods, these bacterial strains metabolize the sugars into energy through a process called glycolysis, which subsequently produces lactic acid as a by-product. It is this specific acidic microenvironment within the oral cavity that sets the stage for tooth enamel demineralization, leading ultimately to tooth decay, a condition medically known as dental caries.
Moreover, the metabolizing of sugars by these bacterial strains accelerates the production of extracellular polysaccharides, primarily glucans. The glucans, in tandem with other bacterial biofilm components, form dental plaque, a colorless, sticky substance that coats the tooth surface. The presence of dental plaque in an acidic environment accentuates demineralization, thereby catalyzing the occurrence of cavities.
Additional insight derives from observational and experimental evidence relating to frequency and timing of sugar consumption. Studies illustrate that frequent exposure to dietary sugars exacerbates acid production and subsequent tooth decay, with the process intensifying during nocturnal hours due to reduced saliva flow, the natural mouth’s defense against acidifying environments.
Also noteworthy is the profound influence of saliva in the sequence. Saliva, laden with calcium and phosphate ions, tends to neutralize the acid, encouraging enamel remineralization. However, persistent acid production, primarily from high sugar consumption, could overwhelm this buffer capacity of saliva. Consequently, the balance tilts unfavorably towards demineralization and ultimately tooth decay.
This interplay between sugars, oral bacteria, and the consequent dental health challenges underscores potent points of intersection for advancing oral health. It advocates for maintaining a symbiotic oral environment where dietary choices optimize the resident oral bacteria’s beneficial qualities while inhibiting pathogenic strains. The essential role of dietary regulation in oral health, especially moderating sugar consumption, thus arises from a well-grounded scientific basis. In conclusion, understanding and navigating these complex biological dynamics is paramount for the continuous progress in preventive dentistry.
Role of Saliva and pH in sugar induced dental problems
Exploring the Interplay of Saliva, pH, and Sugar-Induced Dental Damage
Dentistry’s status quo has been riveted upon the pivotal role of salivary pH in the escalation of detrimental sugar-induced dental decay. This intricate relationship sheds light on how oral health hinges on a delicate balance. Comprehending this underpins real-world preventive measures to maintain our armor against the onslaught of acidogenic bacteria.
Saliva is the unsung hero, not just a passive fluid but an active participant in the oral cavity’s commencement and cessation of the demineralization-remineralization equilibrium. Exceptional attributes such as buffering capacity and mineral resupply capabilities render it indispensable. Yet, the interplay is confounded when saliva encounters dietary sugars, specifically sucrose, which instigates bacteria such as Streptococcus mutans and Streptococcus sobrinus to release lactic acid.
The salivary pH drastically dips in the face of this lactic acid onslaught, creating an environment suited for demineralization – the precursor of dental caries. As a response, saliva attempts to neutralize and reestablish pH stability. However, a constant sugar attack compounded with periods of diminished salivary flow (xerostomia) undermines this. Consequently, the threshold is breached where saliva’s remedial efforts are outpaced by acid’s deleterious effects, setting the stage for dental caries.
The effect of pH variations within the oral environment merits further exploration. As we delve deeper, we turn our gaze to the biochemical puzzle’s intricacies phrased as the Stephan Curve, a graphical representation of the salivary pH fluctuations post sugar intake. This dip-and-rise model illustrates the rapid decline of pH post sucrose-intake and its subsequent, gradual return to baseline.
Furthermore, the pH critical point at which enamel starts to undergo demineralization is approximately 5.5 – a statistic which underscores the significance of maintaining a balanced oral pH spectrum. Shrewd manipulations of sugar intake, ideally limiting fermentable carbohydrates and including non-sucrose sweeteners in dietary practices, could potentially dampen the Stephan curve’s steep falls.
Moreover, saliva’s role extends beyond acting as a buffer. It exerts remineralizing influence aided by calcium, phosphate ions and proteins like statherin. Given their copious presence in saliva, an acid-neutral environment allows combining these ions with the tooth enamel, fostering repair.
Additionally, focusing on enhancing salivary flow could further this cause. Stimulating saliva secretion through chewing sugar-free gum or through pharmacological interventions promotes a more conducive oral environment for enamel remanent.
In conclusion, the interplay between saliva, pH, and sugar-induced dental damage is exceedingly complex. A combined strategy addressing sugar intake, pH regulation, and enhancement of salivary flow might hold the key to reducing dental caries incidence. However, additional studies are instrumental in corroborating these findings and crafting superior dental healthcare strategy. This serves as an earnest testament to our quest for detangling the oral ecosystem’s intricacies in the brave endeavor of preventive dentistry.

Impact of Sugar on tooth enamel and leads to tooth decay
The role of saliva as a protective measure within the oral ecosystem is intrinsic and profound. This dynamic biological fluid acts as a first line of defense against harmful microbes and serves an essential function in maintaining oral health. However, when an individual indulges in high sugar consumption, the salivary pH is significantly disrupted—a factor instrumental in the onset of dental decay.
The relationship between saliva, pH, and dental decay is multilayered. An equilibrium point exists where the oral environment is neither overly acidic nor heavily alkaline, contributing to optimum oral health. This particular pH is considered neutral, around 7, and the further away from this equilibrium, the more challenges the oral health faces.
A model that brilliantly outlines this relationship is the Stephan Curve. Labelling the correlation between sugar consumption, salivary pH, and the duration after eating, this curve demonstrates how the pH in an individual’s mouth drops rapidly straight after consuming sugar, to a degree that can potentially lead to enamel demineralization. Following this dip in pH, the curve suggests a slow return to the healthier neutral roundabout, depending on several factors, such as the quantity and nature of sugar consumed, as well as the initial salivary pH.
The dropping pH level, below the critical point of 5.5, marks the phase where tooth enamel starts crossing into demineralization territory, the point of no return, where it begins losing crucial minerals. This occurs as the acids, produced by bacteria through sugar metabolism, begin to dissolve the Hydroxyapatite crystals, found in enamel, thereby causing damage and, ultimately, tooth decay.
Be that as it may, all hope is not lost, as the sequence is not always irretrievably one-sided. Our saliva carries out a heroic remineralization process, where it deposits lost minerals back onto the enamel to repair the damage. The minerals, like calcium and phosphate ions present in saliva, accelerate enamel repair through this process.
One effective strategy to preserve oral health by maintaining the pH within a balanced range is by promoting salivary flow. An individual can optimize salivary flow by reducing the intervals between meals while incorporating foods that stimulate saliva into their diet. Additionally, habits like maintaining good oral hygiene, regular use of fluoridated toothpaste, and reducing sugary food intake contribute to better oral health.
This multifactorial interplay of saliva, pH, and sugar-induced dental damage is one of the quintessential aspects of oral health. The equilibrium, when maintained, could keep the oral ecosystem thriving. However, disruption, especially through high sugar diets, contributes significantly to the onset of dental decay.
Optimal oral health can be potentially achieved through a combined approach of maintaining salivary flow, regulating sugar intake, and maintaining an overall healthier lifestyle. There exists a palpable need for further research to explore these correlations deeply. A more comprehensive understanding of these mechanisms could revolutionize preventive dentistry, promoting more effective dental healthcare strategies and shifting the focus from treatment to prevention.
Our understanding of the implications of our dietary inclinations, particularly sugar, on dental health lends us the knowledge to adopt healthier practices. The biochemical reactions, role of saliva, pH balance, and consequential impacts on our enamel underline the necessity to maintain a balanced sugar intake and an impeccable oral hygiene routine. It all boils down to the consumption and metabolization of sugar, which can lead to formidable issues if not mitigated by timely and adequate strategies. We can positively contribute to our oral health, ensuring a healthier, happier, and cavity-free future, by understanding and acting upon this detrimental domino effect of sugar on our teeth.